
Schizophrenia (Psychosis) – Novel Solutions to an Old Problem

DR ARUNA
Holistic Psychiatrist
For this month, I decided to write about Schizophrenia – a complex illness that has baffled many great minds throughout history of medicine and psychiatry.
What is Schizophrenia?
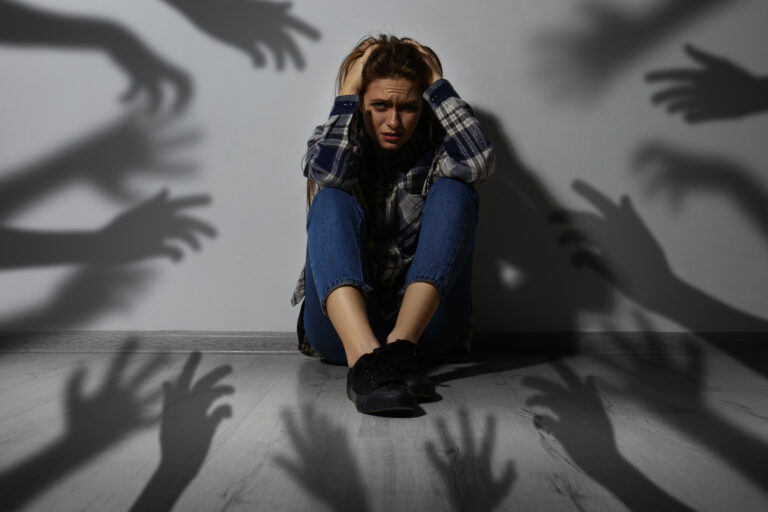
So, what is schizophrenia? It is a serious mental illness that typically affects people during their teen years or early adulthood. Being female appears to be protective for reasons not clearly understood yet. Characteristic symptoms are classified into positive symptoms like: delusions (holding false beliefs) and hallucinations (experiencing sensations in different modalities without any external stimulus – for example hearing voices even when there is no source for the voice); and negative symptoms like memory problems, a severe loss of interest in people, activities and inability to experience emotions and feelings.
Looking at this rap sheet, it is obvious that schizophrenia can wreak havoc in people’s lives. When in active illness, patients are unable to function in many areas of life – work, interpersonal…even self-care can be disrupted.
For ease of delivering my message, I am grouping all psychosis together under the term, schizophrenia – this includes schizophrenia, bipolar disorder, brief psychosis, and all other psychotic states. I am doing this intentionally as my understanding is that the underlying root causes are similar.
What Causes Schizophrenia? New Hypotheses Have Emerged...
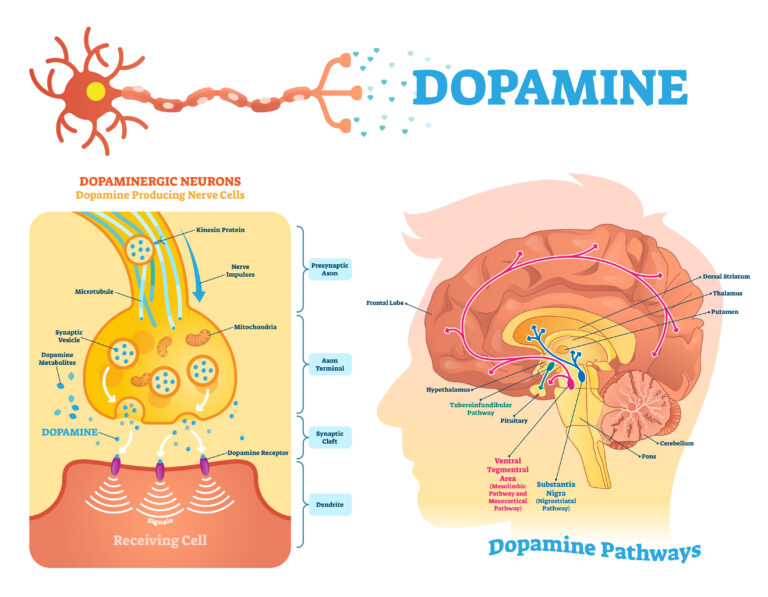
As research has progressed, so has our understanding about what causes schizophrenia. For most of 20th century it was thought to be a result of chemical imbalance, mainly dopamine imbalance. Mainstream psychiatry’s treatment approach is a result of this chemical imbalance hypothesis. It is focused on antipsychotic medications as a mainstay for any psychotic illness. This group of medications are designed to modulate (mainly reduce) dopamine transmission in key areas of the brain; based on the underlying assumption that too much dopamine causes hallucinations and delusions. This theory does not explain the negative symptoms of schizophrenia at all. In fact, we see negative syndrome exacerbating under the effect of these medications.
If dopamine deficiency was the end-all and be-all of schizophrenia; we should expect that these medications will restore dopamine function and thus cure people or at least reduce the positive symptoms of schizophrenia such that the patients experience a good quality of life, can get back to work, and enjoy relationships and life in general.
So, what’s the verdict on the use of antipsychotics for schizophrenia and other psychotic illnesses? Unfortunately, Antipsychotics as a class, have failed to deliver on these expectations (reference 1). Long term studies show that these drugs do not improve recovery rates. On the contrary, they increase disease morbidity, rates of disability, and even cause many chronic physical illnesses (diabetes, hypertension, hyper-cholesterolemia, stroke, heart disease and so, understandably, early death) (references 2,3,4,5,6,7,8).
There is also the problem of “super-sensitivity psychosis” and “tardive dyskinesia” and other tardive movement disorders (references 9,10,11). Tardive means delayed. Dyskinesia and other movement disorders can develop after a few months or after a few years of antipsychotic medication use. They can be triggered by ongoing use or by withdrawal of the medication. Tardive movement disorders are chronic, debilitating, unrelenting, diseases that occur from sustained damage to key dopamine producing areas of the brain. These disorders result in more disability and are typically also associated with “super-sensitivity psychosis” – a term which denotes worsening of psychotic symptoms due to the presence of highly sensitive dopamine receptors in the brain.
Hey, wait a minute, what happened here?
The idea was to reduce the dopamine transmission by blocking various dopamine receptors with these anti-psychotic medications. This does happen and even transient symptom relief is obtained. However, our brain (and body) adapts to the presence of this foreign molecule aka antipsychotic. Long term administration of antipsychotic medications results in chronic dopamine receptor blockage. In response, over time, the brain cells are actually making and manifesting many, many more dopamine receptors. So that even small amounts of dopamine in the brain can stimulate these highly sensitive receptors. Such dopamine receptor stimulation is hypothesized to be the reason behind the tardive movement disorders and the worsening of psychosis. Hence the term, “super-sensitivity psychosis.” In this process, cholinergic neurons (group of neurons that use acetylcholine as the neurotransmitter) also seem to degenerate and become dysfunctional, possibly contributing to TD and possibly even cognitive deficits (reference 12).
The manifestation of these super-sensitive Dopamine receptors also accounts for worsening or emergence of psychosis when patients abruptly stop taking their meds. So it may not be that the original disease is coming back when meds are stopped. It could actually be that the disease was made worse by the use of these medicines.
Clearly, our existing model and treatment methods are not working. We have to go back to the drawing board and see what we have missed. Such critical thinking has paved the way to relatively new hypotheses regarding schizophrenia.
One of them is that the underlying problem could be unchecked and chronic inflammation. There are many evidences that point to the role of inflammation – from presence of inflammatory cells, markers, oxidative stress in the brain, to association with maternal viral infection during pregnancy, to concurrent high risk for “co-morbidities” like auto immune diseases and infections (references 13-24; As you can see this field is exploding with valuable research).
It is only since beginning my education in integrative and functional medicine (where diseases are seen as physiological breakdown in the whole mind-body system) that I am recognizing “chronic inflammation” as the root cause of many modern illnesses.
Another root cause is emotional and personal trauma that can trigger psychotic symptoms as a defense mechanism. But today’s blog is narrowly focused on inflammation. I will, however, say that even emotional trauma, manifests and wreaks havoc by causing inflammation in the brain-body system. So, you see, there is no way to escape the inflammation hypothesis.
The Role of Inflammation
Let me explain a bit more about inflammation. Inflammation is simply the body’s defense and repair response. For instance, when we injure ourselves – say a cut or bruise happens, the area becomes red, swollen, hot and painful. This response to injury is the inflammation response. And this kind of inflammation is time limited. The inflammation repairs the injury and when this repair is complete, inflammation stops. However, when the same inflammation becomes chronic, we then begin to see collateral damage upon various organ systems in the body.
So, what triggers or maintains the inflammation? Chief triggers for chronic inflammation are our lifestyle and diet. Today’s lifestyle is more stress inducing to all ages. The rat race, materialism, isolation, social disconnection coupled with social media addiction, disconnection with nature and natural rhythms of life; are all contributory.
In regards diet, SAD (the Standard American Diet) is pro-inflammatory and filled with artificial frankenfoods. Studies have shown that artificial chemicals in our food and even excess salt and sugar found in processed foods can disrupt the lining of our intestines thus beginning inflammation in the gut. Next, potential triggers are the chemicals in our food system as well in everyday items we use – shampoos, toothpaste, detergent, fragrances, room fresheners, and the list goes on. These chemicals did not exist in our environment pre WWII and our mind-body systems are failing to cope with them. Especially when our detoxification systems are not supported with a nutrient dense diet or because of genetic defects, like the methylation genes, chiefly MTHFR gene (more on this in a later article).
So, it follows that if we address the root cause, which is inflammation, we could potentially experience benefit, maybe even reduction in symptoms and recovery from the illness!
Since implementing this approach, I can safely and confidently say, “Yes, this works!”
Granted, in my private practice, I do not see too many patients with schizophrenia. But I did work with psychosis patients when I worked for a FQHC (Federally Qualified Health Care) clinic that served uninsured, indigenous patients in the community. My experience there re-affirmed my observations that schizophrenia, bipolar disorder and other psychotic states are not a result of a chemical imbalance; but that they are a result of a complex process that implicates systemic inflammation, nutritional deficiencies, detoxification impairments, trauma – real or perceived threat to one’s identity and existence, other socio-economic factors, etc.
A narrow medication-centric approach is a disservice to these patients. Not only because it does not address the whole problem but also because long term studies (there are many that prove this point. One book that has clearly documented all these studies is, Anatomy of an Epidemic, by Robert Whitaker) point to the fact that disability and psychopathology is more prominent in people that stay on these medications long term.
Hence, it is highly imperative that a comprehensive mind-body-spirit-society program is created for each individual struggling with psychosis.
One point I would like to clarify is that the antipsychotic medications do provide symptom relief in the short term. One can make a case for using them in a cautious, judicious manner to gain the benefit of symptom relief while never losing focus on addressing the underlying physiological and psychological root causes. In my practice, I have done both. Started someone on a low dose medication regimen just to get a handle on the symptoms, while implementing a comprehensive root cause resolution program, then judiciously tapering it off as the person recovers. On the other hand, I have also treated patients simply using the Ayurveda based holistic program in my clinic; and have witnessed great results. As in the case of this young woman here.
The Story of One Woman's Remarkable Recovery
I met her for the first time in April 2020. She came in with a diagnosis of schizophrenia and was hospitalized a couple of times. She was prescribed antipsychotics but gained a lot of weight and it did not help with the voices fully. She stopped taking her medications and she would be fine for a while before relapsing with “voices”.
She saw 7 different psychiatrists before me and was always told that she has schizophrenia, she will be ill for her whole life and she has to take the medications long term. (Playing the devil’s advocate, it is not the fault of the psychiatrists here. It is the fault of the medical system that teaches this misinformation, while being slow to keep up with current research). She felt utterly hopeless. After yet another flare up of voices while not on medication, she decided to see me after finding me online.
When I first saw her, what struck me right away was the severe Rosacea she had on both her cheeks. The inflammation inside her body was literally visible on her body, for all to see!! If only, someone made that connection. She was also highly anxious. As I began my interview and I listened to her experience of her symptoms and then her whole life story, I realized that she was actually struggling with severe OCD (obsessive compulsive disorder) and the voices were obsessive auditory images. She did not have insight into them all the time and there were definitely times when she could not distinguish the voices from real perception and fully believed what the voices were saying leading to paranoia. This means that besides the OCD, she would also vacillate into psychosis often – hence, I suppose, the diagnosis of schizophrenia for her.
To confirm my findings, I spoke to her husband and also with her mom to obtain their observational impression of her. From all these accounts, I was convinced about OCD with psychosis as being her primary diagnosis. This may seem like a semantic exercise to the reader 😊. But it is important to be clear about the “form” of the psychopathology as it can help direct treatment. For eg; if it is OCD, I will recommend ERP (Exposure and Response Prevention) as opposed to CBT for psychosis.
Regardless, we needed to delve into the physiological root causes. Once again, leaky gut, food sensitivities and systemic inflammation were at the core of her illness. I explained my hypothesis to this young lady and her family. They were cautiously optimistic as not only did I change the diagnosis, but I had also changed the treatment plan and the prognosis. What convinced them was the unified hypothesis that functional medicine and Ayurvedic medicine gave for all her symptoms. From my vantage point, I saw no reason for her to NOT recover and lead a fully functioning and happy life.
However, the proof is in the pudding, right? So, let’s see what she did…
She was excited and motivated and began the comprehensive diet, supplement, lifestyle plan I recommended. Given the severity of her illness, I had impressed upon her the need for total adherence to the plan.
Gradually, her Rosacea subsided (significantly!). Her skin is not angry looking as before. Her anxiety has subsided, her mood is great. She does not feel depressed anymore. She is eating and sleeping well, enjoying her life again. She has normal energy to take care of her 2 young kids. Most importantly, her voices are gone. Obsessions and intrusive thoughts are also significantly reduced. In fact, I did not even have to refer her to ERP therapy for her OCD. I have continued to provide supportive therapy, education about her illness/symptoms, even shared a rudimentary information about ERP. However, simply taking care of her inflammation, is doing the trick. She is using the CES (cranial electrical stimulation) device, Alpha-stim, which has helped her anxiety and insomnia tremendously.



As part of her work up, we also found that she has Hashimoto’s thyroiditis. We are addressing this problem as well with Ayurvedic herbal medicines and fine tuning her diet even more. She is also recommended Panchakarma, Ayurvedic cleanse treatment, which will remove endogenous and exogenous toxins, and will rejuvenate her whole mind-body system.
Interestingly, she consulted with a traditional endocrinologist for her Hashimoto’s. As I had predicted, the endo doctor basically said there is nothing to do until her TSH increases and T3/T4 is decreasing. Then, she will be put on thyroid medication to supplement her dying thyroid. Once again, Trinergy’s Ayurvedic/functional medicine approach is diametrically opposite. We are looking at the root cause (inflammation), identifying and removing the drivers of it (diet and lifestyle), and providing what her body needs to repair, regenerate and rejuvenate (nutrients, anti-inflammatory and thyroid rejuvenating herbs, Panchakarma detoxification, etc).
Like with our other Hashimoto’s patients, we are confident, that this young woman will also fully recover and have a healthy, functioning thyroid gland forever. Her progress so far is a testament to this fact!
As mentioned before, I never started her on psychiatric medications. She was not keen on taking any med due to her personal history of side effects with them in the past. If her psychosis had not responded, I may have been tempted to prescribe them to ease her suffering. The simple fact is, I did not have to. Within a few weeks of changing her diet and taking our supplements, her symptoms subsided.
The Trinergy Way
So, to recap, here is our solution to her problem:
Reduce inflammation by prescribing an anti-inflammatory diet.
Nutritional Supplementation. Targeted nutritional supplementation was provided to address nutritional deficiencies and also to help reduce the underlying inflammation (references 25, 26).
Regular psychotherapy. Family therapy, supportive therapy, education about her illness/symptoms, etc, were all part of the therapeutic input.
CES device: She is using Alpha-stim on a daily basis to help with her anxiety and insomnia. Alpha-stim is a cranial electrical stimulation (CES) device that when used, provides a tiny amount of electric current to her brain and puts it in the alpha state. Alpha state is the brain’s awake but relaxed state. She reported dramatic improvement in her OCD symptoms since beginning the use of this device. Alpha-stim is a portable device and it is self-administered.
Current status (as of October 2020 at time of writing this article): Free from OCD, psychosis (voices and paranoia), anxiety. Improved energy, mood and vitality. Significantly improved Rosacea (see before and after pictures above).
Our work is ongoing: I expect her to continue to progress in her recovery.
Bottom line: Recovery is possible!
Given that psychosis (and schizophrenia) is a complex and devastating illness, we need to look at all possible solutions to help people with this disease. Integrative Psychiatry seems to offer new hope as it strives to explore the reason (the “why”) people become ill and address those causes.
References:
1. https://pubmed.ncbi.nlm.nih.gov/2021/ 2. https://pubmed.ncbi.nlm.nih.gov/3591992/ 3. https://pubmed.ncbi.nlm.nih.gov/7496641/ 4. https://pubmed.ncbi.nlm.nih.gov/7496642/ 5. https://pubmed.ncbi.nlm.nih.gov/1574549/ 6. https://pubmed.ncbi.nlm.nih.gov/22340278/ 7. https://pubmed.ncbi.nlm.nih.gov/25066792/ 8. https://pubmed.ncbi.nlm.nih.gov/16787887/ 9. https://pubmed.ncbi.nlm.nih.gov/1677263/ 10. https://pubmed.ncbi.nlm.nih.gov/7904833/ 11. https://pubmed.ncbi.nlm.nih.gov/28360793/ 12. https://pubmed.ncbi.nlm.nih.gov/7904833/ 13. https://pubmed.ncbi.nlm.nih.gov/31620871/ 14. https://pubmed.ncbi.nlm.nih.gov/28575316/ 15. https://pubmed.ncbi.nlm.nih.gov/26359903/ 16. https://pubmed.ncbi.nlm.nih.gov/26988846/ 17. https://pubmed.ncbi.nlm.nih.gov/19930265/ 18. https://pubmed.ncbi.nlm.nih.gov/28304340/ 19. https://pubmed.ncbi.nlm.nih.gov/21134972/ 20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3896922/ 21. https://pubmed.ncbi.nlm.nih.gov/29448179/ 22. https://pubmed.ncbi.nlm.nih.gov/29635418/ 23. https://pubmed.ncbi.nlm.nih.gov/16469941/ 24. https://pubmed.ncbi.nlm.nih.gov/30122288/ 25. https://www.ncbi.nlm.nih.gov/pubmed/20124114 26. https://www.ncbi.nlm.nih.gov/pubmed/28823721